Abstract
Polycythemia vera (PV) is characterized by elevated red cell mass due to gain-of-function mutations of the tyrosine kinase JAK2 gene. Major causes of morbidity and mortality in PV are venous and arterial thromboses. Risk factors of thrombosis in PV are age > 60 years, previous thrombosis history, and leukocytosis due to increased granulocytes (PMID: 31865003). High hematocrit has been considered as a causative factor of thrombosis due to high viscosity; however, this has been challenged. Phlebotomy to maintain hematocrit below 45% is performed by most hematologists to prevent thrombosis. However, in our prospective controlled study, we reported that phlebotomies, but not high hematocrit, are associated with increased risk of thrombosis in Chuvash erythrocytosis (CE). CE is due to a hypomorphic mutation of the Von Hippel-Lindau (VHL) gene, a negative regulator of hypoxia inducible factors (HIFs) (PMID 289208), leading to augmented HIFs. We hypothesize that repeated phlebotomies may increase the risk of thrombosis in PV.
We reported that HIFs, and some HIFs-regulated thrombotic genes, are upregulated in PV in both granulocytes and platelets, and even more in PV with a thrombosis history (PMID: 32203583). PV patients with mutated JAK2 have lower ferritin, serum iron, transferrin saturation, and increased soluble transferrin receptor levels compared to JAK2-wild type erythrocytosis (PMID: 30042411), indicating that PV patients with JAK2 mutation are more likely to be iron deficiency (ID). Repeated phlebotomies further augment ID, which increases the level of HIF-1 and HIF-2 by inhibiting the principal negative regulator of HIFs, prolyl hydroxylase domain 2 (PHD2) enzyme. PHD2 requires iron as a co-factor (PMID: 18066546). This led us to hypothesize that further increase of HIFs due to phlebotomy-induced ID increases expression of HIF-regulated prothrombotic genes, leading to increased risk of thrombosis in PV.
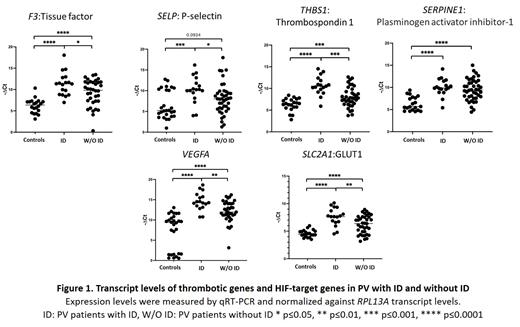
We studied 17 PV with ID, 32 PV without ID, and 19 healthy control and measured their prothrombotic genes' transcript levels in the granulocytes. Of 17 PVs with ID, 9 (56.3 %) had thrombosis while 14/32 PVs without ID (43.8 %) had thrombosis history. We then measured transcript levels of prothrombotic genes, such as F3 (tissue factor), SELP (P-selectin), THBS1 (thrombospondin-1), SERPINE1(plasminogen activator inhibitor-1) and HIF-target genes VEGFA and SLC2A1 (glucose transporter-1). The transcripts of these genes were upregulated in PV with and without ID compared to the controls. However, PV with ID had higher transcripts of these genes compared to PV without ID, except SERPINE1 (Figure 1). These prothrombotic gene transcripts were inversely correlated with ferritin levels and positively correlated with HIF target genes. Thus, ID in PV further augmented HIFs activity and induced expression of prothrombotic genes. In ongoing studies of PV patients serving as their own controls, PV subjects with ID are treated with hydroxyurea to prevent rebound erythrocytosis. The hydroxyurea treatment alone did not normalize high transcripts of prothrombotic and HIF target genes. However, transcripts of these prothrombotic and HIF-target genes decreased after iron correction while their JAK2V617F allele burden did not change.
We then measured transcript levels of these prothrombotic genes in the patients with germline mutations augmenting HIF activity including loss of function VHL, gain-of-function EPAS1 (HIF2a), and loss-of-function EGLN1 (PHD2). These patients have high transcript levels of prothrombotic genes due to high HIF activity although they don`t have ID. Transcripts of F3, SELP, VEGFA, and SLC2A1 of the patients with HIF-pathway mutations were increased compared to the controls and compared to PV without ID but similar to the levels in PV with ID. On the other hand, transcript levels of THBS1 and SERPINE1 in the patients with HIF-pathway mutations were higher than the levels seen in the patients with PV with ID. These data indicate that ID in PV augments HIF activity similar, although not identical, to the patients with germline HIF-pathway mutations and may facilitate propensity to thromboses.
These data suggest that therapeutic phlebotomy to control high hematocrit in PV and other erythrocytoses has the potential to increase thrombosis risk. In our ongoing studies, transcript levels of these prothrombotic genes are being correlated with their functions and protein levels.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal